Coronavirus (SARS-CoV-2) & COVID-19
A dedicated space to inform the public about coronavirus (SARS-CoV-2) and the COVID-19 disease, curated by dedicated members of the Academy.
Coronavirus Background
Historical reference to coronavirus COVID-19 and its presence in the world.
INTRODUCTION
On December 2019, the first acute respiratory syndrome case reports appeared at the Chinese Wuhan municipality, leading to authorities to classify it as a new coronavirus that had not been associated with humans before. As the disease outbreak has quickly spread across China, without the exact source having been detected, has transmitted to a variety of nations in Asian, European, Australian, African, and North American regions, with expected extension to the entire planet.
The novel coronavirus strain and the disease caused by it received an official name on 12 February 2020, becoming the second strain of SARS and labeled as severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), and the disease was referred to as COVID-19. This novel strain of coronavirus, with a confirmed human-to-human transmission, has become a primary concern for public health as there is minimal understanding about its mechanisms of action, its criticality, and possible treatment solutions.
As international health organizations keep close monitoring of the situation and attending to the risks involved, our Academy is honorably dedicated to addressing the event with its expert fellows members as an activity of primordial priority.
RISK ASSESSMENT
Source: ECDC
The main developments since the 2 March 2020 risk assessment can be summarised as follows:
- The 14-day cumulative notification rate of COVID-19, a measure of the prevalence of active cases in the population, is 3.28 per 100 000 population in the EU/EEA as of 11 March, ranging from low rates of <0.1 to 16.3 per 100 000 in Italy and 19.8 per 100 000 in Iceland. The 14-days notification rate increased 10-fold over the last 10 days and, assuming no effect of mitigation measures, the EU/EEA and UK is predicted to reach 100 per 100 000 population (the Hubei scenario) by the end of March.
- While early in the outbreak most cases were reported in China, currently the majority of cases reported are from outside China; and since 2 March, 51% of the cases reported were from EU/EEA countries and the UK.
- There are increasing reports both globally and in the EU/EEA that local transmission has occurred extensively in multiple locations, without reported travel history to areas reporting community transmission and without epidemiological links to known cases [5-8].
- As of 11 March 2020, among the 1 597 cases reported in TESSy where the place of infection was reported, 797 (50%) were reported to be infected in the reporting country, 698 (44%) were reported to have acquired infection in another European country and 102 (6%) had acquired infection outside the EU/EEA.
- In the EU/EEA and the UK, events and locations that involve social interaction or institutional contact have been related to the development of COVID-19 clusters, including workplace interactions, religious events, festivities, health and social care settings, and travel.
- Transmission events have been reported in hospitals, with COVID-19 cases identified among healthcare workers and patients [9,10] as well as in long-term care facilities. As of 9 March, an ongoing outbreak of COVID-19 at a long-term care facility (LTCF) with 120 residents in Washington State (United States) has had 54 residents transferred to local hospitals and 26 deaths, of which 11 were within the facility. Of the 15 that died in hospital, 13 had tested positive for COVID-19. Additionally, 70 of 180 LTCF employees reported symptoms compatible with COVID-19 [11]. In a LTCF in Île-de-France region, France, as of 10 March, authorities report an outbreak of five cases among residents, including two deaths [12].
- Reports from some healthcare facilities in northern Italy indicate that intensive care capacity has been exceeded due to the high volume of patients requiring ventilation [13].
- The Director General of the World Health Organization declared COVID-19 a global pandemic on 11 March 2020.
CHRONOLOGY
Source: ECDC
- On 31 December 2019, the Wuhan Municipal Health Commission in Wuhan City, Hubei province, China, reported a cluster of 27 pneumonia cases (including seven severe cases) of unknown aetiology, with a common reported link to Wuhan's Huanan Seafood Wholesale Market, a wholesale fish and live animal market [1].
- The market was closed down on 1 January 2020. According to the Wuhan Municipal Health Commission, samples from the market tested positive for novel coronavirus. Cases showed symptoms such as fever, dry cough, dyspnoea; radiological findings showed bilateral lung infiltrates [2].
- On 9 January 2020, the China CDC reported that a novel coronavirus (later named SARS-CoV-2, the virus causing COVID-19) had been detected as the causative agent for 15 of the 59 cases of pneumonia [3]. On 10 January 2020, the first novel coronavirus genome sequence was made publicly available [4]. The sequence was deposited in the GenBank database (accession number MN908947) and uploaded to the Global Initiative on Sharing All Influenza Data (GISAID). A preliminary analysis showed that the novel coronavirus (SARS-CoV-2) clusters with the SARS-related CoV clade and differs from the core genome of known bat CoVs.
- By 20 January 2020, there were reports of confirmed cases from three countries outside China: Thailand, Japan and South Korea [5]. These cases had all been exported from China.
- On 23 January 2020, Wuhan City was locked down – with all travel in and out of Wuhan prohibited – and movement inside the city was restricted [6].
- China changed the case definition several times during the course of the outbreak, which caused uncertainty regarding the exact number of cases and the extent of the spread of the virus, and several EU/EEA countries have modified their testing strategies during the course of the outbreak to test only symptomatic or severe cases.
- The first European case was reported from France on 24 January 2020. This case had a travel history to China [7]. In Germany, cases were reported on 28 January, related to a person visiting from China [8].
- On 30 January 2020, the World Health Organization (WHO) declared this first outbreak of novel coronavirus a ‘public health emergency of international concern’ [9]. During the following weeks, several countries implemented entry screening measures for arriving passengers from China [10]. Soon, several major airlines suspended their flights from and to China [11]. Several countries repatriated citizens living in Wuhan.
- A large number of cases have been diagnosed on board the Diamond Princess, a cruise ship docked in the port of Yokohama, Japan. The first cases were reported on 4 February 2020; the ship was put in quarantine.
- As of 3 March 2020, 705 cases have been identified among the ship’s passengers. Of these cases, six died. [12]
- On 22 February, the Italian authorities reported clusters of cases in Lombardy and additional cases from two other regions, Piedmont and Veneto. Over the following days, cases were reported from several other regions. Transmission appears to have occurred locally, in contrast to first-generation transmission from people returning from affected areas. Transmission events were also reported from hospitals, with COVID-19 cases identified among healthcare workers and patients [13]. During the following week, several European countries reported cases of COVID-19 in travellers from the affected areas in Italy, as well as cases without epidemiological links to Italy, China or other countries with ongoing transmission [13]
Since ECDC’s fifth update on novel coronavirus published on 2 March 2020, the number of cases and deaths reported in the EU/EEA has been rising, mirroring the trends seen in China in January-early February and in northern Italy in late February. If this trend continues, based on the quick pace of growth of the epidemic observed in China and northern Italy, it is likely that similar situations may be seen in other EU/EEA Member States.


Geographic distribution of COVID-19
Learn about which locations are affected and view graphical representations of epidemiological curves.
Live Updates COVID-19 CASES
-
 World
?
World
Confirmed: ?
Active: ?
Recovered: ?
Death: ?
World
?
World
Confirmed: ?
Active: ?
Recovered: ?
Death: ?
😷 Global Stats
| Country | Confirmed | Recovered | Death |
|---|---|---|---|
 Worldwide Worldwide |
0 |
0 |
0 |
COVID-19 GLOBAL STATISTICS
Loading....
| Country | Confirmed cases | Death cases | Recovered cases |
|---|

Questions & Answers
The most relevant questions about the disease COVID-19 caused by the SARS-CoV-2 coronavirus.
MEDICAL INFORMATION
What symptoms does a COVID-19 infection present?
Coronavirus can make anyone sick regardless of their age, sex, race or ethnicity.
The virus can cause mild, flu-like symptoms such as:
- Fever
- Dry cough
- Difficulty breathing
- Muscular pain
- Tiredness
- Pneumonia in both lungs
With or without the emergency warning signs including:
- Difficulty breathing or shortness of breath
- Persistent pain or pressure in the chest
- New confusion or inability to arouse
- Blueish lips or face
In addition to cough, fever and shortness of breath, there may be nonspecific symptoms such as sore throat, myalgia, fatigue, nausea, and diarrhea as initial symptoms in some cases.
What treatments are there for the COVID-19 disease?
Healthcare providers are focused on treating clinical symptoms, including difficulty breathing, fever, cough, tiredness, and muscle pain. As the severity of the disease intensifies, implementing therapy for oxygenation, as well as other protocols for supportive care can be of high efficiency.
When to test for COVID-19?
Your current location will address the outbreak differently, depending on its stage at the epidemiological curves and will provide different options both for testing and for other medical attention services. Circumstances will pave way for nations differently as testing and healthcare protocols are adapted to local capacities and needs.
According to the ECDC, "national authorities may decide to only test subgroups of suspected cases based on the national capacity to test, the availability of necessary equipment for testing, the level of community transmission of COVID-19, or any other criteria. As a rational approach, national authorities may consider prioritising testing in the following groups:
- hospitalised patients with severe respiratory infections;
- cases with acute respiratory infections in hospital or long-term care facilities;
- patients with acute respiratory infections or influenza-like illness in certain outpatient clinics or hospitals in order to assess the extent of virus circulation in the population;
- elderly people with underlying chronic medical conditions such as lung disease, cancer, heart failure, cerebrovascular disease, renal disease, liver disease, diabetes, and immunocompromising conditions"
Where can someone get tested for COVID-19?
In case you find yourself presenting symptoms of COVID-19, do not hesitate to contact you local healthcare services by email, chat or by telephone. Further medical testing may be conducted if your healthcare provider finds a reason to and will guide you on the procedure of attention.
Who is more at risk?
Elders and people with other current medical conditions such as cancer, diabetes, chronic respiratory disease, cardiovascular disease, and hypertension, for example, are at a greater risks of presenting severe symptoms.
What is the risk for children?
Evidence of COVID-19 in children have been documented to be mild and rare, as a Chinese study explains, where only 2% of the cases were under 18 years of age. The study addresses the fact that fewer than 3% of the people in the same study developed severe or critical disease.
What is the risk for women during pregnancy?
There is no evidence that the foetus carried by a pregnant woman infected with COVID-19 would be affected, meaning that the mother would not transmit the virus to the baby. Additionally, there are no evident differences suggesting pregnancy will increase the severity of the disease.
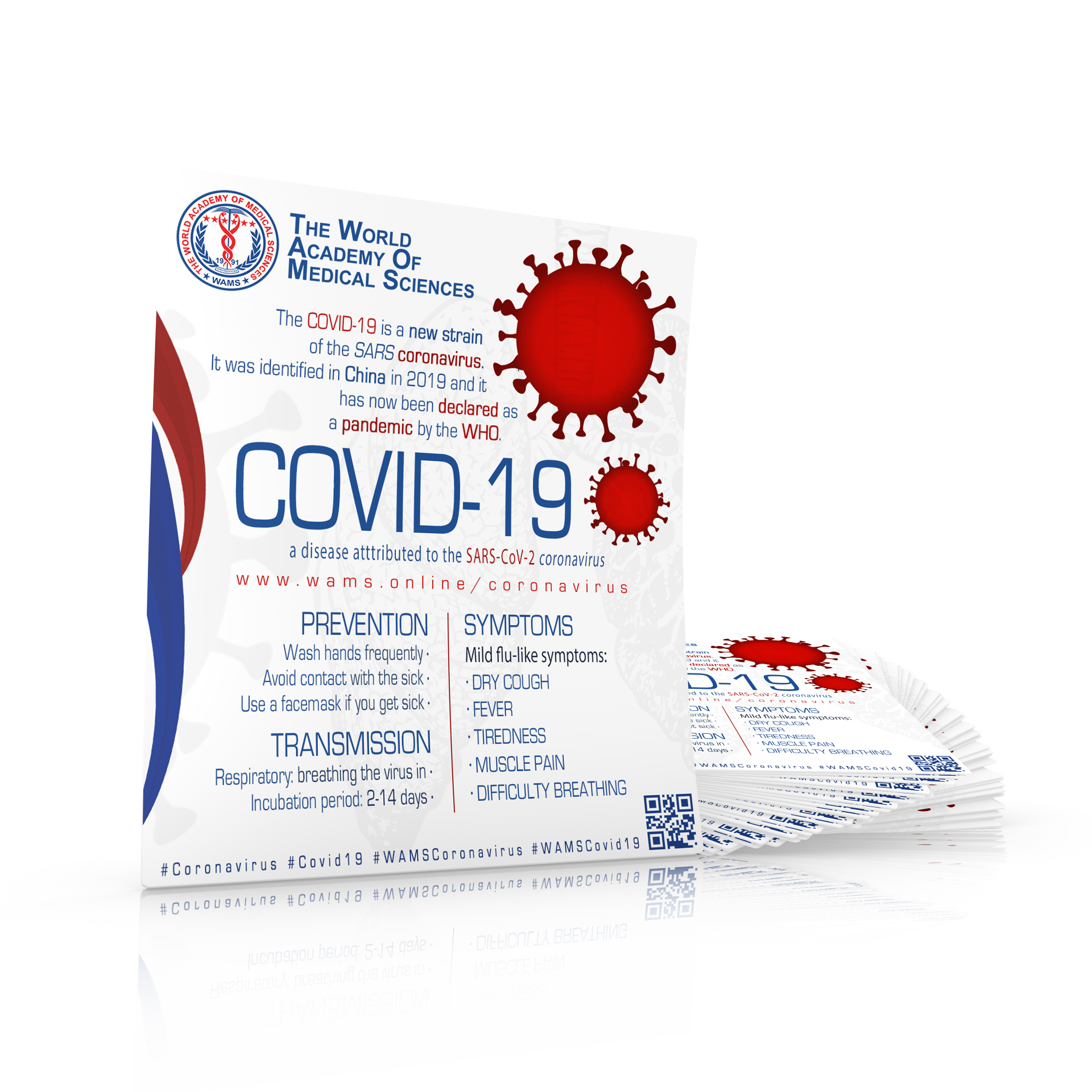
WAMS INFOGRAPHIC ON COVID-19
This infographic provides basic information on novel coronavirus disease (COVID-19), how it spreads, symptoms, how to avoid catching or spreading the virus, and other useful details.
PREVENTION
You can help stop COVID-19 by knowing the signs and symptoms:
Seek medical advice if you have fever, cough or shortness of breath after having been in close contact with a person known to have COVID-19 or if you live in or have recently been in an area with ongoing spread of COVID-19.
What to do to prevent getting infected by COVID-19?
Simple things you can do to help keep yourself and others healthy:
- Wash your hands often with soap and water for at least 20 seconds or use with alcohol-based solutions, gels or tissues.
- Hand wash should be done perforce after blowing your nose, coughing, or sneezing, after going to the bathroom and before eating or preparing food.
- Avoid touching your eyes, nose, and mouth with unwashed hands.
- Stay home when you are sick and remain at least a metre away from others infected.
- Cover your cough or sneeze with a tissue, then throw the tissue in the trash.
What to do if you have been in close contact with people that have COVID-19?
People who have been in close contact with a person known to have COVID-19 or people who live in or have recently been in an area with ongoing spread are at an increased risk of exposure. Notify public health authorities in your location to be able to receive proper attention and directions on how to proceed best.
If you develop any symptoms, you should immediately call your healthcare provider for advice, mentioning that you have been in contact with someone with COVID-19.
MYTH BUSTERS
What can face masks do to protect against COVID-19?
If you are infected, the use of surgical face masks may reduce the risk of you infecting other people, but there is no evidence that face masks will effectively prevent you from being infected with the virus. In fact, it is possible that the use of face masks may even increase the risk of infection due to a false sense of security and increased contact between hands, mouth and eyes.
What efforts are being done to develop a vaccine?
There are currently no vaccines against human coronaviruses, including the virus that causes COVID-19. This is why it is very important to prevent infection and to contain further spread of the virus. The United States FDA is working with vaccine developers and other researchers and manufacturers to help expedite the development and availability of medical products such as vaccines, antibodies, and drugs to prevent COVID-19.
The development of vaccines takes time. Several pharmaceutical companies are working on vaccine candidates. It will, however, take months or years before any vaccine can be widely used, as it needs to undergo extensive testing to determine its safety and efficacy.
What protection does the influenza vaccine have against COVID-19?
Influenza and the virus that causes COVID-19 are two very different viruses and the seasonal influenza vaccine will not protect against COVID-19.

Safety Measures when travelling
Source: ECDC (European Centre for Disease Prevention and Control) - COVID-19
SAFETY MEASURES WHEN TRAVELLING
What precautions should I take if I am visiting an area of local or community transmission?
Travellers visiting areas of local or community COVID-19 transmission should adhere to strict hygiene measures, wash hands with soap and water regularly, and/or use alcohol-based hand sanitisers. Touching the face with unwashed hands should be avoided. Travellers should avoid contact with sick persons, in particular those with respiratory symptoms and fever. It should be emphasised that older people and those with underlying health conditions should take these precautionary measures very seriously.
What if I have recently been in an area of local or community transmission?
Travellers returning from areas of local or community transmission should monitor their health for 14 days. People with symptoms should contact their healthcare specialist via telephone first, and indicate their exposure and travel history before seeking medical attention in person. Symptomatic people should avoid contact with others until they have received advice from a healthcare specialist.
What is the risk of infection when travelling by plane?
If it is established that a COVID-19 case has been on an airplane, other passengers who were at risk (as defined by how near they were seated to the infected passenger) will be contacted by public health authorities. Should you have questions about a flight you have taken, please contact your local health authority for advice. The risk of being infected on an airplane cannot be excluded, but is currently considered to be low for an individual traveller. The risk of being infected in an airport is similar to that of any other place where many people gather.
Why are people not being checked for COVID-19 at the airport when arriving from areas of local or community transmission?
There is evidence that checking people at the airport (known as entry screening) is not very effective in preventing the spread of the virus, especially when people do not have symptoms. It is generally considered more useful to provide those arriving at airports with clear information explaining what to do if they develop symptoms after arrival.
Where can I learn more?
Each EU/EEA country may issue specific advice to travellers to areas with local or community transmission of COVID-19. Consult your local health authority or the Ministry of Foreign Affairs to get advice tailored for residents in your setting.
For an updated list of areas of presumed community transmission, please refer to WHO situation reports for country classification.

COVID-19 AND ANIMALS & FOOD PRODUCTS
What is the risk of COVID-19 infection from animals or animal products imported from affected areas?
There is no evidence that any of the animals or animal products authorised for entry into the European Union pose a risk to the health of EU citizens as a result of the presence of COVID-19.
What is the risk of COVID-19 infection from food products imported from affected areas?
There has been no report of transmission of COVID-19 via food and therefore there is no evidence that food items imported into the European Union in accordance with the applicable animal and public health regulations pose a risk for the health of EU citizens in relation to COVID-19. The main mode of transmission is from person to person.
What is the risk of COVID-19 infection from contact with pets and other animals in the EU?
Current research links COVID-19 to certain types of bat as the original source, but does not exclude the involvement of other animals. Several types of coronaviruses can infect animals and can be transmitted to other animals and people. There is evidence that companion animals (e.g. dogs or cats) have a risk of infection when in close contact with COVID-19 infected humans. As a general precaution, it is always wise to observe basic principles of hygiene when in contact with animals.

National information resources for the public on COVID-19
EUROPE:
| Country | Institute | Website | National helplines |
|---|---|---|---|
| Austria | Federal Ministry Republic of Austria: Social Affairs, Health, Care and Consumer Protection Federal | sozialministerium.at | +43 800 555 621 |
| Belgium | Federal Public Service: Health, Food Chain Safety and Environment | info-coronavirus.be | +32 800 14689 |
| Bulgaria | Ministry of Health | mh.government.bg | +359 2 807 87 57 |
| Croatia | Croatian Institute of Public Health | hzjz.hr | +385 91 468 30 32; +385 99 468 30 01 |
| Cyprus | Ministry of Health | moh.gov.cy | +357 1420 |
| Czech Republic | Ministry of Health | mzcr.cz | +420 724 810 106; +420 725 191 367 |
| Denmark | Danish Health Authority | sst.dk | +45 72 22 74 59 |
| Estonia | Ministry of Social Affairs | koroonaviirus.ee | +372 634 6630; +372 634 1220 |
| Finland | Finnish institute for health and welfare | thl.fi | +358 295 535 535 |
| France | Government of the French Republic | gouvernement.fr | +33 800 130 000 |
| Germany | Federal Ministry of Health | bundesgesundheitsministerium.de | +49 30 346 465 100 |
| Greece | National Public Health Institute of Greece | eody.gov.gr/ | +30 210 521 2054 |
| Hungary | Hungarian Government | koronavirus.gov.hu | +36 6 80 277 455; +36 6 80 277 456 |
| Iceland | Directorate of Health | landlaeknir.is | +354 544 4113, 1700 |
| Ireland | Health Service Executive | hse.ie | +353 1850 24 1850 |
| Italy | Ministry of Health | salute.gov.it | +39 1500 |
| Latvia | Centre for the Prevention and Control of Diseases | spkc.gov.lv | +371 67387661 |
| Liechtenstein | Government of Liechtenstein | regierung.li/coronavirus | +423 230 30 30 |
| Lithuania | Ministry of Health | sam.lrv.lt | +370 8 618 79984 |
| Luxembourg | Ministry of Health | msan.gouvernement.lu | +352 8002 8080 |
| Malta | Government of Malta | deputyprimeminister.gov.mt | +356 21324086 |
| Netherlands | National Institute for Public Health and the Environment | rivm.nl | +31 800-1351 |
| Norway | Norwegian Institute of Public Health | fhi.no | +47 815 55 015 |
| Poland | Government of Poland | gov.pl | +48 800 190 590 |
| Portugal | Ministry of Health | dgs.pt/corona-virus | +351 808 24 24 24 |
| Romania | Ministry of Health | ms.ro | +40 800 800 358 |
| Slovakia | Public Health Authority of the Slovak Republic | uvzsr.sk | +421 917 222 682 |
| Slovenia | Government of Slovenia | gov.si | +386 31 646 617; 080 1404* |
| Spain | Government of Spain | mscbs.gob.es | Regional numbers are found here |
| Sweden | Public Health Agency of Sweden | folkhalsomyndigheten.se | +46 113 13 |
| Switzerland | Federal Office of Public Health | bag.admin.ch/novel-cov | +41 58 463 00 00 |
| UK | Government of UK | gov.uk | 111 (dialled from UK) |
References
- Wuhan City Health Committee (WCHC). Wuhan Municipal Health and Health Commission's briefing on the current pneumonia epidemic situation in our city 2019 [updated 31 December 2019, 14 January 2020].
- European Centre for Disease Prevention and Control (ECDC). Risk assessment: Outbreak of acute respiratory syndrome associated with a novel coronavirus, Wuhan, China; first update 2020 [updated 22 January 2020]. Stockholm: ECDC; 2020.
- Xinhuanet. Experts claim that a new coronavirus is identified in Wuhan 2020 [14 January 2020].
- Holmes E. Initial genome release of novel coronavirus 2020 [14 January 2020]. Available from: http://virological.org/t/initial-genome-release-of-novel-coronavirus/319.
- World Health Organization. Novel Coronavirus (2019-nCoV) SITUATION REPORT – 1, 20 January 2020. Geneva: WHO; 2020.
- Du Z, Wang L, Chauchemez S, Xu X, Wang X, Cowling BJ, et al. Risk for transportation of 2019 novel coronavirus disease from Wuhan to other cities in China. Emerg Infect Dis. 2020 May.
- Santé publique France. Epidémie de coronavirus Covid-19 au départ de Wuhan, Chine. Paris: Santé publique France; 2020. [Cited on 14 February 2020].
- Bayerisches Staatsministerium für Gesundheit und Pflege. Bestätigter Coronavirus - Fall in Bayern – Infektionsschutzmaßnahmen laufen. Munich: BSfGuP; 2020.
- World Health Organization. Statement on the second meeting of the International Health Regulations (2005) Emergency Committee regarding the outbreak of novel coronavirus (2019-nCoV). Geneva: WHO; 2020.
- Phelan A, Katz R, Gostin L. The novel coronavirus originating in Wuhan, China: challenges for global health governance. JAMA. 2020;323(8):709-710. doi:10.1001/jama.2020.1097.
- Chinazzi M, Davis JT, Ajelli M, Gioanni C, Litvinova M, et al. The effect of travel restrictions on the spread of the 2019 novel coronavirus (2019-nCoV) outbreak. medRxiv pre-print.
- European Centre for Disease Prevention and Control. Situation update, 3 March 2020. Stockholm: ECDC; 2020.
- European Centre for Disease Prevention and Control. Outbreak of novel coronavirus disease 2019 (COVID19): situation in Italy – 23 February 2020. ECDC: Stockholm; 2020.

WAMS’ COVID-19 PATIENT MANAGEMENT PROTOCOL
WAMS, the World Academy of Medical Sciences, as the sole official world institution of medical sciences of its kind, puts its principal aim on the task of clearly informing the public and medical audience about the infamous coronavirus COVID-19 (SARS-CoV-2) pandemic and its impact on global human health through its COVID-19 program and through its free digital publication "WAMS' COVID-19 Patient Management Protocol". It brings notice to the characteristics of the phenomenon in various aspects of primordial relevance as an international emergency. This task is being shared among the members of the Academy and its scientific partners across the world with a united spirit of cooperation and dedication to the adequate dissemination of information regarding COVID-19's historical background, geographical distribution, risk assessment, personal health guide, containment & prevention measures, as well as recommendations for public and private sectors to follow.
WAMS Coronavirus Safety Committee
Our dedicated members addressing the pandemic situation.